A new set of HIV Prevention & Accountability reports developed by Frontline AIDS and community partners in India and nine countries in Africa show that while governments have made important progress in reducing the number of people newly acquiring HIV, most are still not investing enough in HIV prevention.
Many governments are still reluctant to make much-needed changes to remove barriers to prevention methods and treatment for those most affected by HIV, including men who sex with men, transgender people, sex workers, people who use drugs and adolescent girls and young women.
We have effective tools and approaches to prevent HIV, including condoms, needle and syringe programmes and exciting new prevention technologies. Yet, last year, 1.3 million people newly acquired HIV around the world, with marginalised communities, such as men who sex with men, transgender people, sex workers and people who use drugs, disproportionately affected. Adolescent girls and young women in Africa are also hit hard. A staggering 3,100 girls aged 15-24 in Africa acquire HIV every single week.
Our new HIV Prevention & Accountability reports provide the community perspective to HIV prevention from partners within the Frontline AIDS partnership, the biggest civil society partnership in the world. They reveal that, due to aggressive campaigning by anti-rights groups, some countries have increased the criminalization of LGBTQ+ people and are rolling back HIV prevention essentials, like the provision of sexuality education and condoms to young people.
Additionally, only a minority of the ten countries have new prevention technologies available and funded. The majority of the ten countries need to scale-up the provision of existing HIV prevention technologies, particularly condoms and pre-exposure prophylaxis, or “oral PrEP”, anti-viral drugs used to prevent HIV. Governments also need to put more funding into these vital tools, alongside actions to address issues with supply and access, and must take steps to ensure that prevention programming reaches the most marginalized communities.
To secure more rapid progress towards achieving global HIV prevention targets, countries urgently need to show leadership by investing more in HIV prevention, countering anti-feminist and anti-LGBTQ+ narratives and ensuring that condoms and new HIV prevention technologies are widely available. International action is also needed to mobilise donor funding, increase domestic funding and bring down the cost of game-changing new HIV prevention technologies, which are currently too expensive for many countries to afford.
New HIV prevention technologies
Countries must do more to ensure their citizens have access to new HIV prevention technologies. The reports show that the Dapivirine vaginal ring, which we know provides women and girls with vital protection from HIV, has not yet been registered in 4 of the 10 countries. An injectable, long-acting form of PrEP, known as CAB-LA, has only been registered in 4 of the 10 countries. Yet CAB-LA has been shown to reduce a person’s risk of acquiring HIV by more than 98%.
Alongside speeding up the registration process, countries need to allocate funding to roll-out these technologies or persuade donors to invest in them. Numerous countries still need to adapt their PrEP clinical guidelines to include these new tools, and to build awareness of them among health workers. Publicity materials to create knowledge and demand for these prevention tools are also needed in almost all countries. Cost is also a major barrier, and the companies that have developed these technologies must do more to make them affordable to low and middle-income countries.
Domestic financing for HIV prevention and Abuja Declaration targets
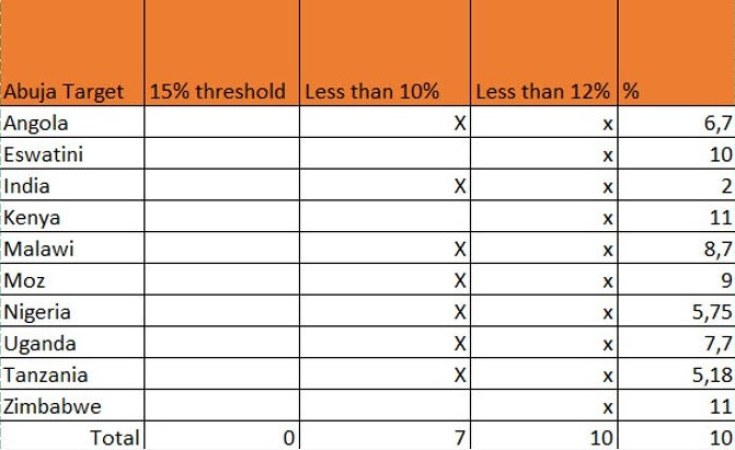
Our reports show that funding from international donors remains the highest contributor to HIV prevention in Africa, especially for programmes aimed at key population communities, such as men who have sex with men, transgender people, sex workers and people who use and inject drugs. Beyond HIV prevention, governments of all nine African countries analysed in our reports are falling far short of meeting the target to spend 15% of their national budgets on health, as set out within the Abuja Declaration.
This reliance on international donors threatens the sustainability of the HIV prevention response, particularly now with international funding for HIV decreasing and a number of donor countries cutting their aid budgets, or reallocating aid to other areas. It also raises questions about each governments’ commitment to ending AIDS as a public health priority.
Rising anti-rights movement
Across the ten countries our research highlighted an organized and well-funded anti-rights movement and anti-LGBTQ+ mobilisation – particularly in Kenya, Tanzania and Uganda – which is rapidly gaining influence. 7 out of 10 countries [have laws that] criminalise people who engage in same-sex sexual acts. This poses a major threat to HIV prevention progress, particularly in Africa.
Uganda has passed one of the world's harshest anti-LGBTQ+ laws that calls for life imprisonment for anyone convicted of homosexuality and prescribes the death penalty for certain same-sex acts. The bill also criminalizes any person who fails to report same-sex acts to the police, meaning that supportive family members of LGBT people could be imprisoned for not reporting their loved ones to authorities. Even before the law had been approved by parliament, it had already generated a surge in human rights violations and had reduced HIV prevention and treatment services for LGBTQ+ people.
Many anti-rights groups are mobilising against the provision of sex education and condoms for young people, as well as against new HIV prevention technologies, with false claims that these approaches will make young people promiscuous.
Despite the worrying rise in anti-rights activity, some countries have taken progressive steps to strengthen HIV prevention efforts and human rights. In Angola for example, the government has decriminalised both same-sex sexual acts and sex work and has prohibited discrimination against people based on their sexual orientation
Frontline AIDS community partners have urged their governments to stand up against anti-rights narratives and to defend HIV prevention services as they are essential for protecting the health and wellbeing of all communities. Despite the challenges, our partners are offering life-saving HIV prevention services to those that need it most, and are advocating strongly to improve HIV prevention in countries around the world.
Abuja Declaration Targets
7 out of 10 countries spend less than 10% of their government budget on health.
None of the 9 African countries is near to meeting their national funding targets of 15% (as set out in the Abuja Declaration in 2001) which raises questions around the sustainability of the response.
Youth focus
Rules on the age of consent for Sexual and Reproductive Health and HIV services are undermining access to HIV prevention for young people. Some are able to access HIV testing, but not HIV prevention commodities or family planning. Across many of the countries, conflicting policies in the health and education sectors also mean that few young people have access to condoms in schools.
9 out of 10 of countries do not allow access to condoms in schools. In only 4 out of 10 countries (Angola, Eswatini, Mozambique and Uganda), adolescents (aged 12+) can access HIV testing without parental consent.
Shrinking civic space
9 out of 10 countries are using laws and policies to restrict civic space. And 7 of 10 countries have passed or tabled new legislation that would further restrict civic space.
Civil society and community organisations play an essential role in the HIV response, particularly in reaching people who face stigma, discrimination or criminalisation, or who are otherwise left behind.
In 7 of the 10 countries, governments have introduced, table or passed new laws that place restrictions on civil society groups. This trend is taking place alongside a rise in government crackdowns on LGBTQ+ organisations and on civil society groups that provide HIV services to LGBTQ+ people. This will impact on their ability to register, access funding and to engage in advocacy and accountability work aimed at strengthening the HIV response.
Prof Nana Poku, Chair of Frontline AIDS, said: “Today’s landmark report shows that while governments across Africa and in India have made important steps towards reducing the number of people newly acquiring HIV, much more can and needs to be done in the fight against HIV.
“Our reports highlight that all nine of the African countries analysed are presently failing to meet the target of spending 15% of their national budgets on health, as outlined in the 2001 Abuja Declaration. With effective tools and approaches to prevent HIV, including exciting new prevention technologies, it is vital that governments take the requisite steps in order to stop more people newly acquiring HIV around the world.
Lois Chingandu, Director of External Relations, Frontline AIDS said: “It is important that countries do more when it comes to investing in HIV prevention methods but also show stronger leadership in countering anti-rights narratives within their countries. Well-funded and highly organized movements are promoting anti-gender expression and anti-LGBTQ+ narratives which have resulted in 7 out of the 10 countries analysed criminalizing people who engage in same-sex sexual acts.
“While progress has been made, barriers to HIV prevention remain. Today’s report highlights the need for further investment to prevent HIV but also much stronger leadership when it comes to countering anti-rights narratives if the global community is to strengthen and progress the HIV response across these nations.”
About Frontline AIDS
Frontline AIDS is the world’s largest partnership of civil society organisations working to end HIV and AIDS. Together, we are working to create a future free from AIDS for everyone, everywhere.
Around the world, millions of people are denied HIV prevention, testing, treatment and care simply because of who they are and where they live. As a result, around 1.3 million people became newly infected with HIV in 2022 and around 630,000 died of AIDS-related illnesses.
Together with partners on the frontline, we work to break down the social, political and legal barriers that marginalised people face and continually adapt and innovate to create a future free from AIDS.
Please visit our website to learn more.