Growing up in the dusty streets of Hurungwe, Juliet Chimedza was her father's trusted sidekick. The father was a well-known traditional healer, famous for 'treating' even the most serious diseases like cancer.
Of course, Juliet learnt all the tools of the trade and she would be sent to dig up some of the roots they used in treating their patients from in and around their village of Kanyati.
Many years later, at 42-years, Juliet had taken over from her father to become a traditional healer herself.
Not once did she think that she would be affected by the very disease she used to 'treat' others of.
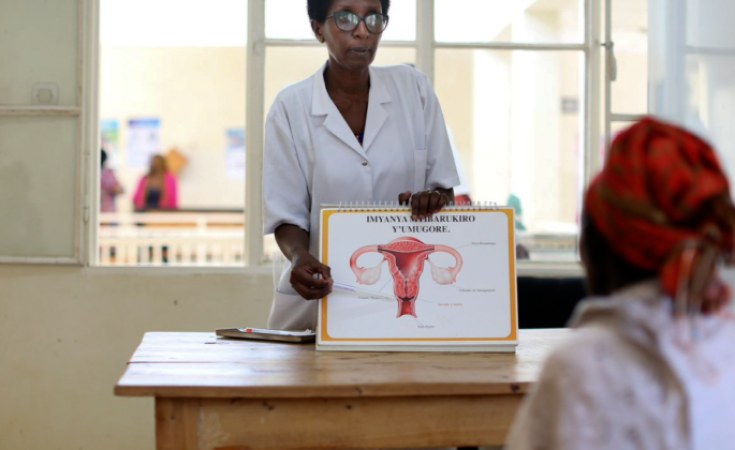
"Last year, a village health worker came to our community and she was educating us about cervical cancer and how they were using a new method to collect samples from women which would then be taken to the lab to test for cervical cancer," said Juliet.
"Out of curiosity, I just took one of the self-testing kits just to see what would happen. I thought to myself, 'I might be treating others when I also have this cervical cancer, so let me just see what happens'," she said.
Unfortunately, when her results came back, they were positive.
She went to Hurungwe Rural District Hospital where she underwent a visual inspection with acetic acid and cervicography (VIAC) screening that confirmed that she indeed had pre-cancerous cells in her cervix. She immediately received treatment.
While Juliet has since given a clean bill of health, hers has been a lesson that anyone can get cervical cancer and screening is important in detecting it early.
HPV is the most common sexually transmitted infection (STI) and can cause six types of cancer, including cervical cancer, the most common cancer among women in Zimbabwe.
According to the National Cancer Registry annual report, cervical cancer accounted for 21 percent of all cancer cases reported in the country in 2018. Among black women in the country, it was the most frequent cancer, accounting for 39,2 percent of all the cases.
Today, on International HPV Awareness Day, Zimbabwe and the world celebrates Juliet and many other women whose lives have been saved by early screening.
The day seeks to raise awareness about the human papillomavirus (HPV) and its associated cancers.
Despite being the most common of all cancers, cervical cancer is also the only HPV-related cancer that can be prevented through vaccination and early detection.
Government, through the Ministry of Health and Child Care (MoHCC), established the National Cervical Cancer Screening Programme in 2012, offering screening and treatment services. The programme has grown significantly since then.
Primary prevention is being carried out through HPV vaccination for girls 9-14yrs while secondary prevention is provided through screening using VIAC and HPV testing for women 25-49.
From June 2023, the Clinton Health Access Initiative (CHAI), in collaboration with the Ministry of Health and supported by the Judith Neilson Foundation and Unitaid, have been working in Mashonaland West province to expand access to cervical cancer screening and treatment models in the province through decentralised screening in the communities using Community Health Care workers.
CHAI supported the Ministry to implement community based self-sampling models as a way to expand screening coverage, while ensuring labs, referral and data systems are strengthened so that screening translates to treatment as needed.
This programme is part of a multi-country grant from Unitaid covering Kenya, Malawi, Rwanda, Nigeria, Zambia and Zimbabwe.
And this is what saved Juliet's life, along with many other women in Hurungwe.
"I believe that this programme saved my life because we always believe that traditional medicines alone can heal us but sometimes you need to get to a health facility to detect a disease. I now encourage people to get screened and I refer most cancer patients to the hospital because we might cause delay while trying to treat something which can easily be treated in a health facility and in the end it will cost us the life of one too many women," said Juliet.
The self-sampling method has resulted in more women getting screened for HPV, despite initial resistance from some members of the communities.
Said Madran Mutami from Muchinjagora village: "When this initiative came, I did not accept it all because I am a member of the apostolic church and I only believed what I was told at church. After some time, I realised that some of the symptoms I was feeling were similar to what the community health workers were saying about cervical cancer so I decided to try the self-sampling. I was relieved when I tested negative but since then, I now encourage other people to always get screened so that they know where they stand."
Although screening is the best way to detect cervical cancer early, many women do not do this owing to long distances travelled to health facilities.
Others also cited reservations about the invasive VIAC process, hence they opted not to go for screening.
"We stay far from the hospital so I could not come for screening only when I did not have any symptoms. We are happy that at least this self-sampling method is easy and it is coming to the village so we do not have to travel long distances," said Mercy Matukanzvimbo from Mutunhu village.
Since the inception of the programme, there has been a rise in the number of women getting screened for cervical cancer.
Hurungwe rural hospital VIAC nurse sister Ngonidzashe Goredema said working with village health workers had made a positive impact as they were closer to the people.
"When we started, we received 100 test kits and from those, 16 tested HPV DNA positive and all these 16 clients came for VIAC services here. Some of them then tested VIAC positive while others tested negative. Those who tested positive went on to receive treatment. To date, we have collected almost 300 samples which have gone to the lab. The number is increasing because we have seen that many women do not like to come in for testing by nurses so they are responding well to this self-sampling method," she said.
The community health workers said although it had been difficult to convince women to take up this screening method, many were now accepting it.
Ms Future Matekenya said: "We have been educating them and telling them that cervical cancer has no sign or symptom that will alert them early on of its existence. So we have ensured that they understand what it is we are trying to do and that the process is simple and free of charge. We also inform them that having precancerous cells is not a death sentence and this can be treated early before it becomes cancer. It was difficult at first but now they have accepted it."
To ensure that the programme is more acceptable, the hospital has engaged local churches as well as traditional leaders to encourage women to get screened.
Chief Nematombo said all village heads under him were part of the programme to ensure that no one was left behind.
"We are thankful for this programme which has come to us where women can take samples themselves and the results come to them without them having to go to a health facility. As chiefs, we work with village heads so that they can mobilise their people and alert them about this programme. Women have been coming and we are happy," he said.
On their part, the churches have tried to involve the men, who are the main carriers of the human papillomavirus.
Pastor Simbarashe Mada from AFM Zimbabwe in Magunje said it was the responsibility of everyone to educate the people about cervical cancer to avoid unnecessary death of women to the disease.
"When we learnt about HPV we realised that men are the carriers so we took this education to our churches. We have been encouraging the men to allow their women to go and get screened so that they can be treated early if they have cervical cancer. We hope to invite those with spouses who are not church members so that we can educate them as well about this disease and protect our women," he said.
Mashonaland West provincial medical director Dr Celestino Dhege said HPV vaccination and early screening were important in the fight against cervical cancer.
However, he said the reach of the VIAC services was limited, hence the self-sampling HPV DNA programme would improve coverage.
"In Mashonaland West the programme was commenced in the last quarter of 2023. One of the reasons was that we would reduce the number of people who need VIAC services considering that our coverage was already limited," said Dr Dhege.
"We have started with 20 sites and we hope to spread it out so that almost all our sites can provide such services to cover all the women."
Dr Dhege said doctors in the province would receive training to perform loop electrosurgical excision procedure (LEEP) which treats abnormal cell growth on the surface tissue of the cervix.
"This is so that the continuum is complete; we screen with HPV DNA, those who test positive proceed to do VIAC and those who may be VIAC positive proceed to receive Cryotherapy and where necessary proceed to receive LEEP," he said.
"We hope this will help to prevent cervical cancer and ensure that our women continue to live longer healthy lives."