June 19th is designated every year to mark World Sickle Cell Day. This international awareness day aims to increase public knowledge and understanding of sickle cell disease, as well as the challenges faced by patients, their families, and caregivers.
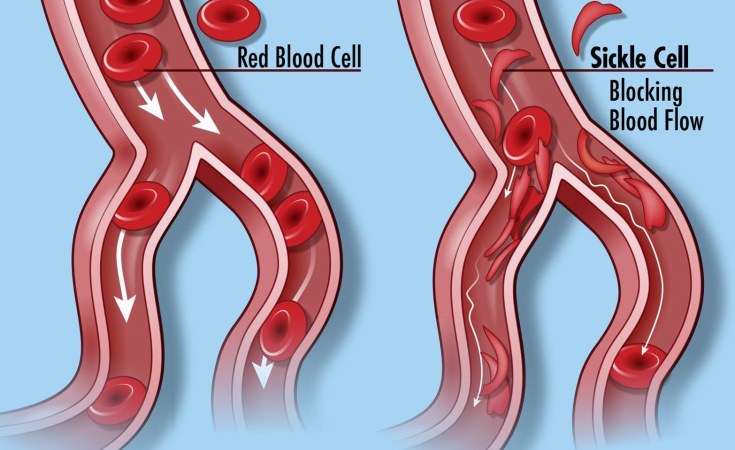
It is important to note that sickle cell disease is a blood cell disorder that causes red blood cells to take on a sickle or moon shape due to an abnormality in the oxygen-carrying protein called hemoglobin. These abnormally shaped cells can stick to vessel walls, blocking the flow of blood and preventing proper oxygen circulation.
As a result, individuals with sickle cell disease do not have enough healthy red blood cells.
People with sickle cell disease are also at risk of complications such as stroke, acute chest syndrome, blindness, bone damage, and priapism.
Over time, individuals with sickle cell disease may experience organ damage to the liver, kidneys, lungs, heart, and spleen. Complications from the disorder can also lead to death. The treatment of sickle cell disease primarily focuses on preventing and managing these complications.
According to reports, Nigeria bears the highest burden of sickle cell disease (SCD) globally and is the top sickle cell endemic country in Africa, with an annual infant death toll of about 150,000, representing more than 8% of infant mortality in the country.
Globally, approximately 50 million people are living with sickle cell disease, with Nigeria being the epicenter and home to about 4-6 million individuals with the disease.
Each year, around 300,000 newly diagnosed sickle cell children are born worldwide, and at least 100,000 babies in Nigeria die from the disorder, making it the number one sickle-cell endemic country in Africa, as per 2014 statistics from the World Health Organization (WHO). These statistics are alarming.
Unfortunately, awareness of sickle cell disease in Nigeria remains abysmally low, with many Nigerians still unaware of the disease, particularly in rural communities.
It is worth noting that testing for sickle cell disease is simple. A genotype test can determine whether a person carries the sickle cell trait (AS), and as long as carriers do not partner with other carriers, none of their children will be born with sickle cell disease.
Sadly, there are reports of couples forging their genotype and phenotype test results to enable them to get married. Medical practitioners usually advise that individuals with the AS genotype should find partners with the AA genotype, as this ensures that none of their children will have sickle cell disease. Despite counseling and warnings, many couples ignore doctors' advice and proceed with marriages.
This newspaper urges the government at all levels to make testing for sickle cell disease mandatory for all newborn babies in hospitals.
This testing should be accessible, free, and compulsory for all aspiring couples and newborns.
The earlier parents or caregivers start managing sickle cell disease, the better the outcomes. Proper management is key.
The government should also double its efforts in spreading awareness of the dangers of sickle cell disease. There should be a clear government policy on sickle cell disease, similar to those for cancer and HIV.
Treatments for sickle cell disease include medication, blood transfusions, and, in rare cases, bone marrow transplants. Bone marrow transplantation involves replacing damaged cells in the body with healthy ones. However, this treatment option is expensive and out of
reach for the common man.
It is gratifying to note that there has been a major breakthrough in the treatment of Sickle Cell Disease (SCD) with the approval of Crizanlizumab by the National Health Service England. The NHS has secured a deal to make this life-changing revolutionary treatment available to up to 5,000 patients over the next three years. With access to this drug, people will experience an improved quality of life, and hospital attendance due to emergency situations will be reduced by 40 percent.
Consequently, efforts should be made by the government, private individuals, and non-governmental organisations to establish bone marrow transplant centers in at least all the geopolitical zones in the country. This would ensure that individuals with sickle cell disease have access to this life-saving treatment option.
Moreover, the government, wealthy private individuals, and corporations can play a vital role in funding research and making financial assistance available for those who cannot afford the breakthrough drug. By investing in research and providing financial support, more affordable treatment options can be developed, ensuring that individuals from all walks of life can access the necessary care.
The government should also take steps to establish sickle cell emergency care centres dedicated to handling sickle cell emergencies.
These specialised centres would provide prompt and effective care for individuals experiencing sickle cell-related complications.
Furthermore, it is important to encourage more healthcare workers to specialise in caring for sickle cell patients. This can be achieved by offering incentives such as scholarships, grants, or additional benefits to those who choose to pursue these specialties. By incentivizing healthcare professionals, we can ensure that there are enough trained experts to provide quality care to individuals with sickle cell disease.